Dramatic treatment effects are rare
Posted on 21st August 2017 by Emma Solyom

This is the twelfth blog in a series of 36 blogs based on a list of ‘Key Concepts’ developed by an Informed Health Choices project team. Each blog will explain one Key Concept that we need to understand to be able to assess treatment claims.
“Breakthrough”, “Wonder Drug”, “Cure”; it’s time to make sense of these headlines.
Few treatments are worthy of such dramatic headlines. So it’s time we start questioning such claims and thoroughly investigating the research behind the headlines. [1]
There are treatments that have dramatic effects…
Treatments with dramatic effects are ones where everyone (or nearly everyone) treated experiences a benefit (or harm). For instance, astounding results are achieved with morphine for pain relief, insulin for diabetes, adrenaline for severe allergic reactions and blood transfusion for shock. In these cases, the benefits of the treatments are obvious, immediate and dramatic: there is little uncertainty that these treatments are effective. [2]
However, treatments producing large, dramatic effects are rare…
Most treatments have smaller, more modest effects. This is not to say that treatments with modest effects are unimportant. But it’s rare that the evidence will be so clear-cut that there’s no room for doubt about whether or not a treatment is effective. Instead, it’s more likely that there will be some uncertainty about how well a treatment works, or whether a treatment could do more harm than good.
Take aspirin for example…
Aspirin is not a cure for heart disease, but it can reduce early mortality after heart attack by a considerable 20%, if given promptly on diagnosis. However in some cases, taking aspirin after a heart attack could do more harm than good. For instance, taking aspirin can increase the risk of stroke and the risk of bleeding from the gut. For a patient with underlying cardiovascular disease, the benefits of taking aspirin are likely to outweigh these risks. But if the individual does not have underlying cardiovascular disease, the risks associated with taking aspirin are likely to outweigh the harms. This highlights the importance of weighing the benefits and risks of treatments and reveals how the benefits of treatments might differ for different people [3].
Indeed, for any given treatment, it is more likely than not that there will be uncertainty about which treatment is best for which patient or that there will be uncertainty about the extent to which treatments work. So what should clinicians and patients do in these circumstances? When we’re uncertain about a treatment effect, we need to refer to the best evidence available.
We need to ask questions like:
- Have there been fair (unbiased) comparison of treatments?
- Are there large trials?
- Are the participants representative of the population? Have they been allocated at random to treatment comparison groups?
- Was there unbiased measurement of treatment outcomes?
- Are the statistical analyses appropriate and have they been correctly carried out?
Putting these points together from a number of different research papers helps form a systematic review – if well done, a trustworthy way to avoid mistaken conclusions. [3] So, ideally, when there’s uncertainty, we should refer to any systematic reviews that exist. But, if there’s still uncertainty after referring to a systematic review, or if a systematic review doesn’t exist, clinicians and patients should discuss this uncertainty, and the different treatment options, together. When there’s a lack of evidence, it’s also researchers’ responsibility to take steps to reduce uncertainty through carrying out well-designed research.
As we’ve just seen, uncertainties about the effects of treatments are common.
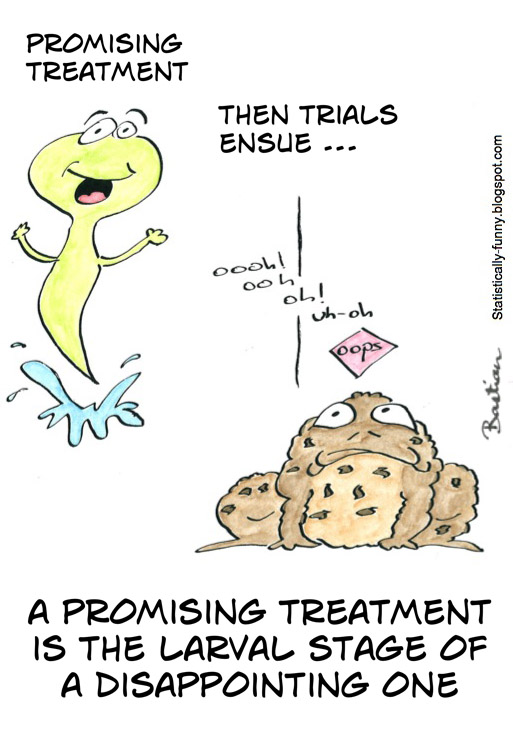
Cartoon with credit to Hilda Bastian: http://www.testingtreatments.org/promising/?nabm=0
So why are claims about treatments sometimes exaggerated and blown out of proportion in the media? Well, in a population instilled with worry and fear, where reports declare that 1 in 2 people will get cancer [4] and many more will be affected by other diseases, it is no wonder that the population’s expectations of science and medicine are increasing. The media emotively reassures and promises great things, and “Breakthroughs” and “Wonder Drugs” are splashed across headlines. [5] But in reality, be aware that such promises are unrealistic and scientific progress is slower.
For instance, after multiple claims that a cure for cancer is within reach, there is still a tremendous amount of research required to achieve this. In the last 40 years, the extremely low survival rate for patients suffering from pancreatic cancer, for example, has not changed. [6] A lot is at stake when publishing results: funding, careers, businesses, time. Positive, ground-breaking results are the aim, and results may be skewed to help suggest that these have been achieved. [7] There is undoubtedly a need to search deep beneath the media reports and public service announcements to pick apart the science that should lie there.
There is definitely a need for greater honesty in the medical world. Publishing papers that are inconclusive or that give unremarkable results is fundamental to the development of science and our understanding. Changes in science and research are gradual and require a step-by-step process. HIV for example was first identified in the 1920s and only now in October 2016 has a possible cure been created; a cocktail of drugs, which are still not fully understood. [8] These changes are not sudden and drastic, but each step requires reliable analysis of data.
For now, we need to be critical about what we’re reading…
After all, not all treatments produce dramatic effects. It’s much more likely for treatments to have moderate, small or trivial effects – and we need to be realistic about this and sceptical about claims of any new ‘wonder drug’.




